
| Blogs
Approaches to implementing hospital-wide electronic document management (EDM) system
< Return to the insights hub
The advantages and disadvantages of different EDMS implementation approaches. If you are about to introduce a hospital-wide electronic document management (EDM) system, there are several implementation approaches to consider. Here, we discuss the different options and their respective pros and cons.
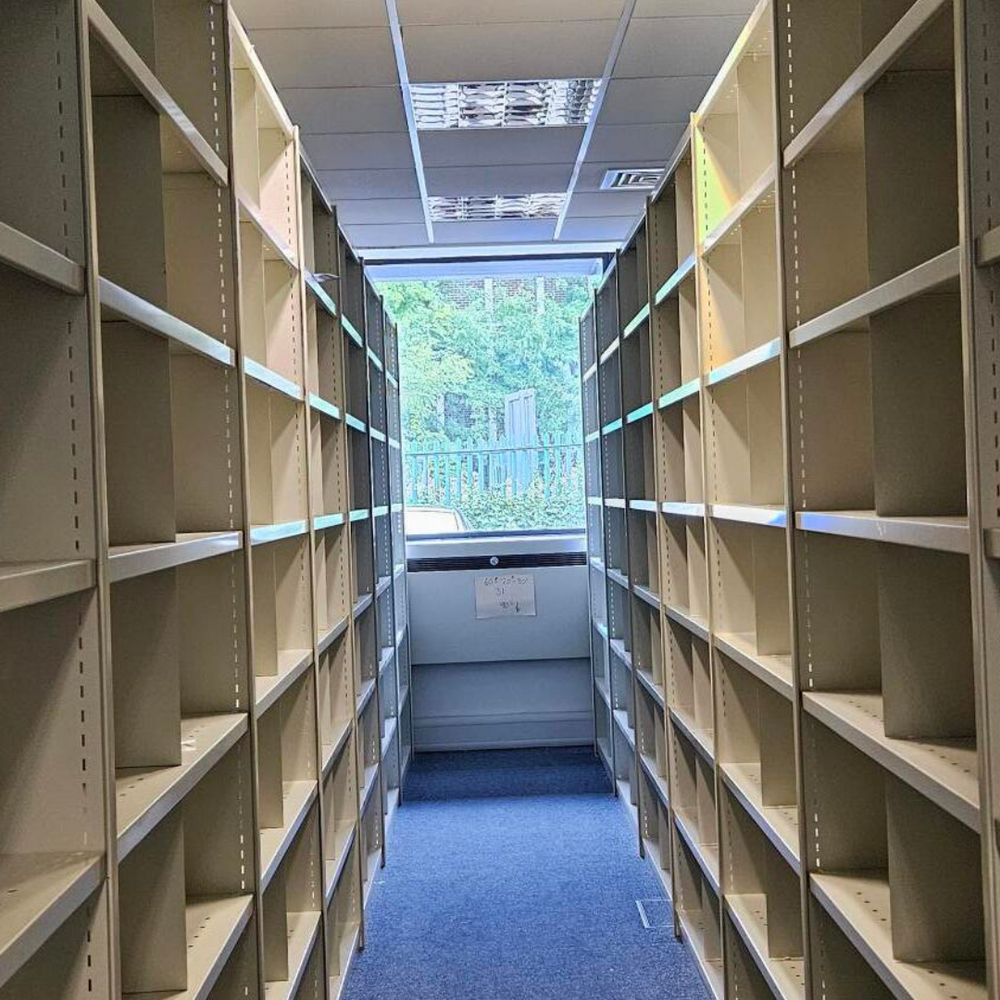
Most NHS Trusts recognise that continuing with paper case notes is unsustainable, if they are to meet service demands. Some may have run out of physical storage space or be looking to realise the many cash-releasing benefits through the closure of a record library.
Yet, regardless of the strategic drivers, which may be significantly different from trust to trust, the overriding consideration will be to ensure that the EDM system will:
Identify and deliver efficiency savings at a departmental level to provide a return on investment;
Provide measurable improvements to patient safety and clinical efficiency – allowing clinicians to mine information easily from scanned case notes and quickly associate documentation with patient encounters;
Be deployed without having a detrimental impact on departmental operations.
It is important to consider the different implementation approaches and the advantages and disadvantages of each option. This should take into consideration your own business drivers, organisational capability, infrastructure and affordability, so that you evaluate and make recommendations based on the best approach for your organisation.
Your EDMS programme can be split into two sub-projects, albeit with strong inter-dependencies:
Deployment of an EDMS for accessing patient records in a clinical context
Implementation of a scanning service to digitise existing patient case notes and ongoing capture of new patient documentation.
Deployment approaches for EDMS
The three most common implementation approaches tend to be:
Do nothing — Do not implement EDMS
Phased deployment — Deploy EDMS on a speciality-by-speciality basis, using outpatient clinics as the trigger for scanning
Big bang approach — Deploy the EDMS across all clinics in all specialities from the agreed go-live date.
Option 1: do nothing
Advantages
No requirement for additional investment in the short-term, or until additional physical library capacity is needed
Challenges associated with managing organisational change will not be faced.
Disadvantages
Fails to address the needs of the clinician in that immediate access to essential patient information will still not be available without pre-arrangement
Continued risk to security and confidentiality
Physical space constraints will remain at the health records library
Still gives rise to fire and health and safety risks
Not a cost-effective option – resource time is being spent ‘firefighting’ rather than being used efficiently
No significant opportunity to realise benefits with regard to patient safety clinical/information governance, health records department or across the administrative establishment
Fails to address any recommendations of the NHS Information Strategy, Connecting for Health initiatives or meet the Trusts strategic ICT aims
Contrary to the concept of the modern NHS and 2025 paperless target.
Option 2: Phased deployment
Phased deployment can take place on a speciality-by-speciality basis, initially using outpatient clinics as the trigger for scanning. Once the back and forward scanning functions are proven to be stabilised and clinicians across all specialities have been trained on using digital patient records, documents relating to discharge records can also be digitised.
The pace of the phased implementation from initial go-live will be largely dependent upon the following factors:
Availability of Trust training resources to ensure that adequate support is provided to clinicians during go-live
The scanning supplier can continue to meet agreed service level agreements (SLAs) as the volume of records scanned increases in line with the phased speciality roll-out plan
Forward-scanned documentation is being processed in a timely manner
IT equipment (new PCs, mobile devices, additional networking etc.) is installed in clinical areas.
Advantages
A phased deployment allows the organisation to be flexible to ensure scanning services can meet agreed SLAs. Specialities can go live one after the other, or a few at a time, depending on scanning and transformation capacity. In the event of any concerns, pulling data for the next set of clinics can be paused.
Clinical engagement and transformation activities are focused at speciality level, enabling concerns to be easily identified and addressed
Process changes are tested, proven and embedded prior to introducing them in another speciality
Fewer resources are required simultaneously to implement/support a phased deployment
It is still recommended that transformation activities take place across all specialities ahead of go live, to understand the impact of taking physical notes out of circulation.
Disadvantages
The deployment time (between the first and last speciality go live) is greater than with a big bang approach
It may take longer to realise all the associated benefits with a phased deployment
Patient records scanned whilst attending a live clinic will need additional floorwalking support if the patient attends a non-live speciality.
Option 3: Big bang approach
A ‘big bang’ approach enables EDMS to be deployed across all clinics in all specialities from the go-live date. Sufficient time will need to be allocated prior to go-live for transformation activities, and a speciality should be identified as an early adopter in order to verify new processes before deploying hospital-wide.
The success of a big bang implementation will be largely dependent on the following factors:
Having sufficient transformation and support resources to cope with this approach
Ensuring that all transformation activities have taken place across all services to understand the impact of taking physical notes out of circulation
Understanding that the scanning throughput for on-demand and forward scanning will be vast from go-live, therefore SLA’s will need to be closely monitored. If the scanning team fall behind, there is a risk that patients could be referred on or followed up without key information being available to clinicians.
Advantages
Enables a rapid deployment if the transformation and support resources are in place to cope with simultaneous demands on implementation, training, scanning and IT support activities
Benefits can be realised sooner than with a phased deployment
All users will be familiar with the EDMS Solution from go live. This will result in a reduced support requirement if scanned patients move between specialities.
Disadvantages
There is a concentrated resource requirement to support a big bang deployment
The scanning throughput for forward scanning could be significant from go-live. SLA’s will need to be closely monitored
If either scanning team (back and forward scanning) fail to meet SLAs, patients could be seen, referred on or followed up without key information being available. This could cause significant patient safety issues.
As a big bang deployment is not confined to a particular speciality, it is more difficult to pause the on-demand scanning in the event of any issues. This could have a detrimental impact on clinical acceptance and result in a loss of confidence in the programme.
Our recommended approach
A phased deployment is our recommended approach to deploying an EDMS, as it allows for continued verification of operational and scanning processes to ensure SLAs are being met. In the event of any concerns, the subsequent clinics planning to go-live could be paused until resolution.
This implementation approach has proven successful as it has ensured that the EDMS deployment is focused on continually supporting individual clinicians with the transition. This is key for establishing and maintaining clinical engagement throughout the project lifecycle.
We hope that this brief introductory guide will help you to evaluate the optimum approach for your organisation. For more information, please get in touch
We hope that this brief introductory guide will help you to evaluate the optimum approach for your organisation. For more information, please get in touch.
We hope that this brief introductory guide will help you to evaluate the optimum approach for your organisation. For more information, please get in touch.
Related posts

guide
The Challenge of Managing Access Requests in NHS Trusts

guide
Empowering healthcare: A guide to patient-centric digital records in the NHS
guide
Building the economic case for an NHS EDMS guide
case study
Helping Northumbria Healthcare NHS Foundation Trust digitise 1m+ patient records

case study
Barnsley Hospital achieves digital excellence with partners Mizaic, System C and Iron Mountain
case study
Hillingdon Hospitals NHS Foundation Trust transforms healthcare infrastructure

case study
Helping Northampton General Hospital NHS Trust digitise 200,000+ medical records

case study
London North West University Healthcare NHS Trust celebrates 170,000+ digitsed records

event
Digital Health Rewired 2025
